中国科学院微生物研究所,中国微生物学会
文章信息
- 刘子豪, 梁媛, 刘丹, 陈红伟, 杨洪早. 2023
- LIU Zihao, LIANG Yuan, LIU Dan, CHEN Hongwei, YANG Hongzao.
- 根除细菌生物被膜的新视角:分散
- Dispersion: a new perspective for eradicating bacterial biofilm
- 微生物学报, 63(12): 4451-4466
- Acta Microbiologica Sinica, 63(12): 4451-4466
-
文章历史
- 收稿日期:2023-04-13
- 网络出版日期:2023-06-30
2. 国家生猪技术创新中心, 重庆 402460;
3. 西南大学医学研究院免疫学研究中心, 重庆 402460
2. National Center of Technology Innovation for Pigs, Chongqing 402460, China;
3. Immunology Research Center, Medical Research Institute, Southwest University, Chongqing 402460, China
细菌生物被膜(biofilm, BF)是指细菌黏附于生物体或非生物体表面,由蛋白质、胞外DNA (extracellular DNA, eDNA)、多糖等分泌组成的胞外聚合物(extracellular polymeric substances, EPS),因其固着的生活方式和能在胞外形成一种独特且复杂的自我保护结构而表现出与浮游细菌完全不同的特征,能显著提高细菌对宿主免疫系统的先天抵抗力与对外界压力(如饥饿、脱水、抗菌剂等)的耐受性[1-2]。值得注意的是,BF细菌对各种抗菌药的耐药性是浮游细菌的10−1 000倍,且BF是细菌为适应生存环境而形成的一种与浮游细菌相对应的生存形式,一般的消毒剂和抗菌药难以穿透其胞外脂多糖(lipopolysaccharide, LPS)基质层,同时BF具有很强的黏附性,导致清除困难,这使得BF在临床中更易引发难治性慢性感染,严重威胁人类与动物健康,对21世纪医疗保健构成了极其严峻的挑战[3-4]。因此,迫切地需要找到行之有效的治疗方案以改善和攻克生物被膜相关感染(biofilm-associated infections, BAI)。
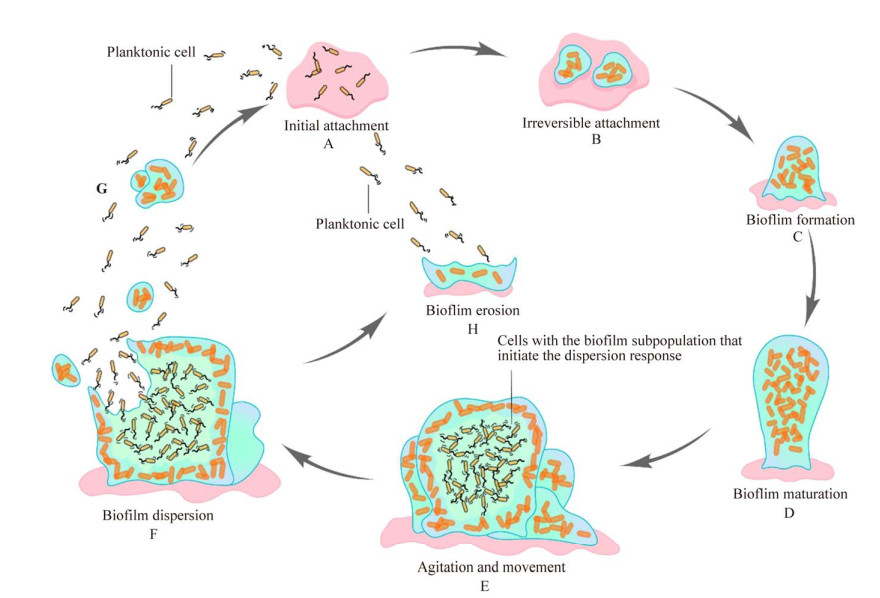
尽管BF结构具有物种多样性,且相同菌种在不同环境条件下也能形成不同结构的BF,如柱状、蘑菇状和微克隆体等[5],但无论物种、条件如何变化,BF的形成与发育阶段均符合一般特征,即BF形成的过程为循环周期(图 1):浮游生物黏附、微菌落形成、BF成熟和BF分散[6]。与细胞受到外界压力被动地离开BF不同,BF分散是一种主动且活跃的事件,其中固着、基质包裹的膜内细胞会主动逃离BF,留下被侵蚀和具有中心空隙的BF,由于它被认为会导致细菌转移到新的定植地点,所以又被称为“播种分散”[7]。也即表明,在BF分散后,膜内细胞会重新恢复浮游状态,而这种状态的细菌耐药能力大幅减弱,更易受到抗菌药和免疫反应的影响[8]。因此,诱导BF分散被认为是一条能控制BAI的新策略。而且,分散行为具有自主性,加速BF行为的产生,而不直接杀灭细菌,也可能避免新耐药问题的产生。但BF为何会自行分散,该如何促使BF分散,通过BF分散治疗BAI的可行性又如何,这些问题均有待深入研究。
|
| 图 1 BF的形成与分散[6] Figure 1 Biofilm formation and dispersion[6]. A: Initial attachment. B: Irreversible attachment. C: Biofilm formation. D: Biofilm maturation. E: Agitation and movement. F: Biofilm dispersion. G: After biofilm dispersion, the cells in the membrane will resume their planktonic state. H: Bioflim erosion. |
本文结合BF分散研究进展及课题组研究基础,对BF分散方式、机制及研发分散剂与其潜在性影响进行了系统的概述,希望能为BAI的治疗提供新思路,并为深入研究BF分散机制奠定理论基础。
1 生物被膜分散方式BF分散是膜内细胞发生主动逃逸的结果。在分散过程中,膜内细胞会自主产生基质降解酶促进分散(如藻酸盐裂解酶、β-N-乙酰葡糖苷酶、分散蛋白B、细胞外DNA酶和糖基水解酶PsIG等)。编码酶的基因是如何被激活,目前尚不明确,但可以肯定分散是在一些信号分子的诱导下发生的,而根据触发分散的不同信号来源,可归为两类:内源性信号分子分散和环境诱导的分散。
1.1 内源性信号分子分散内源性信号分子分散,是为响应细胞自我合成的信号分子或线索而发生的分散,通常源自成熟BF的中心区,可伴随部分细胞亚群的死亡,但存活下来的细胞能逃离BF进入周围环境,在BF内留下大的空腔或空心结构[9]。这说明BF的分散不具有整体性,起源于局部事件,而且发生分散的细胞亚群与BF的直径和厚度也存在联系。通过对流通池中BF细胞的微观观察表明,分散仅发生在最小直径超过40 μm、最小厚度超过10 μm的BF内,即表明当BF体积较小时,信号分子的诱导可能不会引起分散,而且当增大流通池内流体流速与流量时,发生分散的BF体积也在增大(直径、厚度增加)[10]。而介质的流速、流量与BF生长所需物质的运输有关,这也说明BF的持续生长不利于BF的维持。因此,在内部环境逐渐恶劣的情况下,膜内细胞产生了一系列信号分子,帮助自身逃离BF。常见颇具代表性的内源性分散信号分子包括环鸟苷二磷酸(cyclic dimeric guanosine monophosphate, c-di-GMP)、N-酰基-高丝氨酸内酯(N-acyl homoserine lactones, AHLs)、假单胞菌属喹诺酮类信号、脂肪酸信号以及自诱导肽(autoinducing peptide, AIP)。
1.1.1 c-di-GMPc-di-GMP发现于驹形杆菌纤维素合酶的变构激活剂,已被公认为是细菌当中一种无处不在的第二信使,在调控BF形成周期、协调细菌运动性与毒力因子的表达中均起到关键作用[11]。BF细菌通常表现出高水平的c-di-GMP,而浮游菌则表现出低水平的c-di-GMP。c-di-GMP的水平由GGDEF结构域的二鸟苷酸环化酶(diguanylate cyclase, DGCs)和含有内吞体自噬溶酶体(endosomal-autophagic-lysosomal, EAL)或组氨酸天冬氨酸甘氨酸酪氨酸脯氨酸(histidine-aspartic acid-glycine-tyrosine-proline, HD-GYP)结构域的磷酸二酯酶(phosphodiesterase, PDEs)共同调控,DGC催化c-di-GMP的形成,PDE促进c-di-GMP的降解[12]。降低胞内c-di-GMP水平已被认为是根除BF的一种新策略。Elgamoudi等[13]报道,c-di-GMP能抑制空肠梭菌BF形成,并能以剂量依赖性方式分散BF,还能增强空肠梭菌的趋化运动,降低其黏附性。细菌内c-di-GMP水平的降低会导致BF EPS的减少,促进BF分散,如编码双域GGDEF-EAL蛋白的基因dipA或rbdA丢失后,EPS含量会伴随细菌内c-di-GMP水平的升高而不断增加,其中rdba具有明显的pel依赖性[14];研究还发现ΔrbdA突变体中pelA基因的表达量增加了1.5倍,EPS的形成明显增多,而ΔdipA突变体不仅多糖增多外,还表现出群体运动力的降低和初始附着能力的增强[15]。类似的PDE还有YfiN、MucR、NbdA、RpfR、Bifa、RmcA和MorA等[16-17]。因此,可通过调节PDE降低细胞内c-di-GMP水平以促进BF分散。
此外,对于c-di-GMP作用的研究大都集中于革兰阴性菌,在革兰阳性菌中也发现具有相似的作用,只是目标和监管机制可能有所不同。对于此2类细菌BF共性的研究,将有利于加深对BF的理解,如抑制淀粉样蛋白聚合、糖苷水解酶和脱氧核糖核酸酶对基质组分的降解都可能会影响该2类的BF形成。
1.1.2 AHLsAHLs是由革兰阴性菌产生的一类自诱导剂(autoinducer, AI),也是最经典的一类信号分子[18]。AI是群体感应(quorum sensing, QS)调节的产物,能参与BF形成的多个阶段,如基质合成、流体通道、柱状结构形成以及BF分散[19]。涉及BF分散的AHL包括N-3-氧代十二烷酰高丝氨酸内酯(N-3-oxododecanoyl homoserine lactone, 3-O-C12-HSL)、N-丁酰基-l-高丝氨酸内酯(N-butyryl-l-homoserine lactone, C4-HSL)和7, 8-顺式-N-十四烯酰基高丝氨酸内酯等[20-21]。
3-O-C12-HSL和C4-HSL是铜绿假单胞菌QS系统LasI/LasR和RhlI/RhlR的产物,LasI/LasR系统能正向调节与BF形成相关的酪氨酸磷酸酶A (tyrosine phosphatase related to biofilm formation A, TpbA)的合成,TpbA不仅能抑制基因pel表达,还能使c-di-GMP水平降低,引起BF分散,其中pel基因参与调节EPS中胞外多糖EPS的合成,而EPS合成需要c-di-GMP与受体PelD的结合[22-23]。其中C4-HSL已被证实可通过上调鼠李糖脂(rhamnolipid, RL)的生物合成基因rhaA诱导BF分散,RL是一种产自铜绿假单胞菌的BF表面活性剂,对BF的形成至关重要,适量的RL是初始微菌落形成的必需物质,还能维持BF结构稳定,但过量RL则会极大地促进BF分散[24]。还有研究发现,RL能诱导其他菌种BF分散,如Wood等[25]使用铜绿假单胞菌PA14上清液(RL为主要成分)分散了98%工业污染菌硫酸盐还原细菌(sulfate reducing bacteria, SRB)的BF;Bhattacharjee等[26]利用铜绿假单胞菌的培养基,诱导了大肠埃希菌BF分散,可能是3-O-C12-HSL和RL产生协同作用的结果,RL通过改变大肠埃希菌BF对AHL的选择通透性,使得3-O-C12-HSL诱导BF分散。
1.1.3 喹诺酮类信号2-庚基-3-羟基-4-喹诺酮(Pseudomonas quinolone signaling, PQS)是铜绿假单胞菌产生的另一种AI,也称为喹诺酮假单胞菌信号[27]。PQS信号早前因能够介导铜绿假单胞菌BF中细胞的死亡和EPS中eDNA的释放,而引起关注。随着研究的深入,PQS系统逐渐被认为是Las I/Las R和Rhl I/Rhl R系统外的第三大QS系统,并作为前两大系统的调节剂发挥作用,PQS可以通过正向调节RL的合成产生C4-HSL,而诱导BF分散[28]。PQS系统的主要组分包含2-庚基-4-羟基喹啉(2-heptyl-4-hydroxyquinoline, HHQ)、2-庚基-3-羟基-4-喹诺酮(2-heptyl-3-hydroxy-4-quinolone, PQS)、2-庚基-4-羟基喹啉N-氧化物(2-heptyl-4-hydroxyquinoline N-oxide, HQNO)、转录调节因子PqsR和PQS效应元件PqsE,其中只有PQS充当信号分子,并表现为一种多功能分子[29]。Lin等[30]认为在c-di-GMP低水平下,PqsR可介导pqs和rhl表达,促进绿脓菌素和RL合成,诱导BF分散。除了调节其他QS系统外,PQS还能介导外膜囊泡(outermembrane vesicles, OMV)形成、铁的获得和细胞毒力因子表达等,其中OMV同时包含具有蛋白酶活性、脂肪酶活性以及DNA酶活性的酶,进而显著促进BF分散[31]。
1.1.4 脂肪酸信号与BF相关的脂肪酸信号通常指的是可扩散信号调控因子(diffusiblenal factor, DSF)家族信号,因其2位的顺式不饱和双键是关键活性结构特征,所以DSF信号都属于顺式不饱和脂肪酸[32]。DSF家族信号被认为是一种新的QS系统,参与一系列生物学功能的调节,如细胞生长、BF发育、毒力因子表达等。
DSF作为顺式-11-甲基-2-十二烯酸首次被发现于黄单胞菌中,其合成依赖于RpfF-RpfB双组分系统,当细菌密度较低时,RpfF合成的DSF较少,RpfC因难以感知DSF而保持未磷酸化,与RpfF结合形成复合物,限制DSF合成;当细胞密度较高时,DSF分子积聚,RpfC能通过跨膜传感器结构域感知并与其结合,在组氨酸激酶结构域内自磷酸化,释放RpfF,促进DSF合成[33]。磷酸化的RpfC能将磷酸转移至RpfG激活PDE活性,降低c-di-GMP水平,激活c-di-GMP响应性转录调节因子CLP,与manA和xag启动子结合,促进内切β-1, 4-甘露聚糖酶的释放和抑制xagABC基因表达,导致EPS减少,引发BF分散[34]。其他诱导BF分散的DSF信号还包括反式-2-癸烯酸(trans-2-decenoic acid, SDSF)、顺-2-癸烯酸(cis-2-DA)和顺式-2-十二烯酸(BDSF)等[35]。综上所述,或许能将DSF家族信号作为药物靶标研究其成为抗菌药的增效剂,以控制BAI。
1.1.5 AIPAIP是由葡萄球菌、链球菌、芽孢杆菌等革兰阳性菌产生的一类AI,已被证实能引起辅助基因调节系统(accessory gene regulator, agr)介导下的BF分散[36]。Agr由AgrD、AgrB和双组分信号传导系统AgrC-AgrA组成,AgrD负责合成AIP前体(Pre-AIP),AgrB对Pre-AIP进行修饰并将其转运到膜外与AgrC结合,接着AgrC在组氨酸残基处发生自磷酸化,然后将移至AgrA处的磷酸化AgrC激活,磷酸化的AgrA能进一步激活酚可溶性调节肽和细胞外蛋白酶的表达,并抑制BF基质蛋白,如纤连蛋白结合蛋白(fibronectin-binding proteins, FnBPs)和蛋白A等的合成,从而引起BF分散[37]。
1.1.6 其他分散信号除上述经典的内源性分散信号外,更多的信号分子也逐渐被发现,如霍乱自诱导因子-1 (cholerae autoinducer-1, CAI-1)与AI-2通过协同作用可促进霍乱弧菌BF的分散[38];过磷酸化的鸟嘌呤核苷酸(guanosine pentaphosphate/tetraphosphate, (p)ppGpp)在营养胁迫下诱导恶臭假单胞菌的BF分散[39];RNA噬菌体Qβ复制酶的宿主因子(host factor for RNA phage Qβ replicase, Hfq)依赖性小RNA (small non-coding RNA, sRNA)能协调淀粉欧文菌BF的分散等[40]。每种信号分子都具有一定调节活性,通过激活特定的信号通路,达到促进BF分散的目的。目前可知,革兰阴性菌、革兰阳性菌及真菌关于BF分散的调控机制是不同的,但在BF基质组成上,三者却有着较大的相似性,这意味着如酶等具有基质降解能力的物质,可能对多个菌种的BF造成影响。
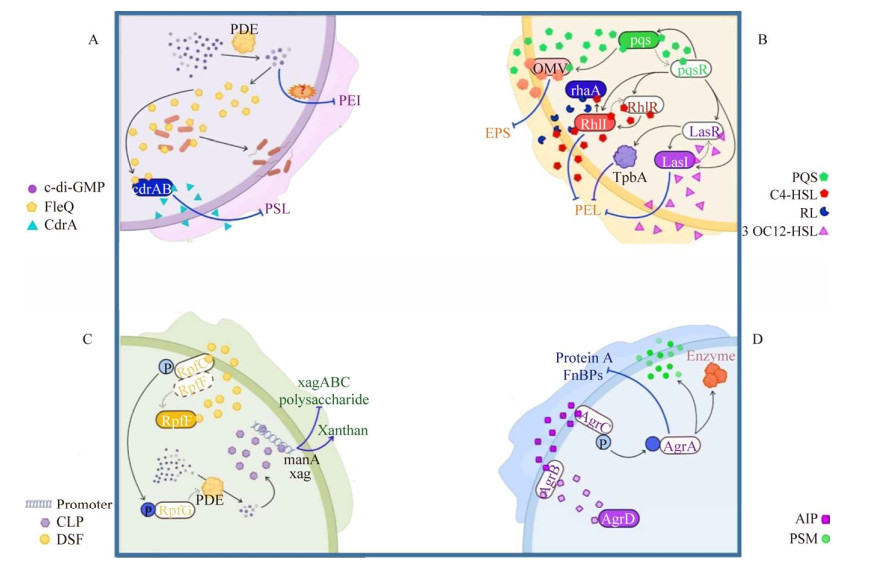
基于此,依据上述介绍的内源性信号分子,绘制了与BF分散相关的4种调控机制通路图(图 2),以此为分散领域的深入研究提供参考。(1) c-di-GMP介导的分散(图 2A):在PDE的作用下胞内c-di-GMP水平降低,低水平c-di-GMP一方面可诱导酶的产生进而降低基因表达,另一方面激活FleQ进而抑制CdrA合成,减少PSL,同时激活鞭毛形成,促进细菌逃逸。(2) AHL信号与PQS信号共同作用导致的分散(图 2B):此通路由LasI/LasR、RhlI/RhlR和PQS系统组成,LasI、RhlI和PQS分别合成QS信号分子3-O-C12-HSL、C4-HSL和PQS,转录因子LasR、RhlR和PqsR分别检测各自的信号分子,形成前馈自诱导回路,并调控靶基因转录;此外,PqsR还正向调控LasI/LasR和RhlI/RhlR,PQS介导OMV表达,抑制EPS形成;LasR促进TpbA表达,与3-O-C12-HSL和C4-HSL一起抑制PEL合成;C4-HSL也能诱导RL形成,从而显著促进BF分散。(3) DSF信号引起的分散(图 2C):在高细胞密度时,RpfC在DSF的刺激下自磷酸化,释放RpfF,并将其移到RpfG,激活PDE活性,降低c-di-GMP水平;低水平的c-di-GMP可增强manA和xag启动子表达,从而减少相应多糖的产生。(4) AIP诱导的分散(图 2D):AgrD合成Pre-AIP,并将其转运到AgrB中,加工成AIP,从而诱导AgrC磷酸化;然后将磷酸化AgrC转移到AgrA上并激活它,从而诱导胞外蛋白酶和苯酚可溶性调节素(phenol soluble modulins, PSMs)的产生,同时抑制蛋白A和FnBPs的形成。
|
| 图 2 BF分散的调控机制 Figure 2 Mechanisms that regulate BF dispersion. A: c-di-GMP-mediated dispersion. B: Dispersion caused by the combined action of AHL signal and PQS signal. C: Dispersion caused by DSF signals. D: AIP-induced dispersion. |
综上所述,各类天然分散信号间可能存在一定联系,但这种相互关联以促进BF分散的调控机制有待深入研究,且目前有关信号分子的机制研究主要基于铜绿假单胞菌等革兰阴性菌,仅有少部分会涉及到革兰阳性菌与真菌,故未来应加大对不同致病菌种BF分散的研究,以此研发出更具有专一性的BF分散剂,为防治BAI奠定理论基础。
1.2 环境诱导的分散信号与内源性信号分子分散不同,环境诱导的分散响应于外界环境的变化,如碳底物的突然增多或减少、NO的导入、缺氧、磷酸盐的可用性降低和铁等微量元素的缺乏等。其中BF内缺氧导致的“还原压力”需要克服丙酮酸入侵[41];磷酸盐作为一种必需的营养素对于核酸的合成和信号传导至关重要[42];铁元素不仅是BF形成中关键酶的辅助因子,还能降低NO分散BF的有效性[43]。因此,降低氧、磷酸盐与铁元素的可用性均能引起BF分散,但其作用机制不明,有待进一步的研究。本文主要概述碳可用性及NO对于BF分散的诱导。
1.2.1 碳可用性碳源是BF形成的主要营养来源,碳底物浓度的突然升高可诱导BF分散。琥珀酸、谷氨酸与葡萄糖都能作为有效的诱导剂触发铜绿假单胞菌BF分散,其中琥珀酸的BF去除量高达80%[44]。类似的情况也发生在肺炎链球菌和白色念珠菌中,葡萄糖底物的增多能诱导小鼠鼻咽部上皮细胞中肺炎链球菌BF分散,500 nmol/L的葡萄糖即能使白色念珠菌的BF显著分散[45]。除碳源增多外,碳源的消耗也被证明能诱导BF的分散。在恶臭假单胞菌中,碳源耗尽时,由(p)ppGpp介导的严谨反应通过正调节磷酸二酯酶和负调节亮氨酸氨肽酶活性(leucine aminopeptidase genes, LapA)及其转运系统进而促进BF分散[39]。在铜绿假单胞菌中,葡萄糖饥饿5 min,BF即开始发生环磷腺苷(cyclic adenosine monophosphate, cAMP)介导的分散,并在24 h时达到60%的分散量[46]。cAMP是一种重要的细胞内信号转导分子,碳源可用性能调节cAMP的产生。在霍乱弧菌中,葡萄糖耗尽时,cAMP与cAMP受体蛋白(cAMP receptor protein, CRP)结合以启动CCR (碳分解代谢物抑制),cAMP-CRP可通过上调HapR表达以引起BF分散,HapR被认为是BF基因表达的一种负调节因子,若该蛋白表达量下调则会显著增强BF形成[47]。此外,碳源的酶促消耗也能诱导BF分散,如丙酮酸脱氢酶(pyruvate dehydrogenase, PDH)能使铜绿假单胞菌的BF量减少71%,金黄色葡萄球菌的BF量减少40%[41]。
1.2.2 一氧化氮一氧化氮(nitric oxide, NO)最早作为细菌厌氧代谢的产物被发现,随后发现内源性NO能诱导铜绿假单胞菌BF分散,并且导入外源性NO可引起多菌种BF分散,如大肠埃希菌、核梭杆菌、黏质沙雷菌和霍乱弧菌等[48-49]。500 nmol/L的供体硝普钠(sodiumnitroprusside, SNP)能使地衣芽孢杆菌的BF量减少90%,10 μmol/L SNP可使表皮葡萄球菌的BF量减少60%[50]。此外,NO还能使白色念珠菌BF减少60%,并在与氯联合处理时可去除废水厂85%−90%的多物种BF[48]。NO引起BF分散的调控机制,也在对革兰阴性兼性厌氧菌(如嗜肺军团菌、霍乱弧菌、铜绿假单胞菌等)的研究中得到了阐释,其调控系统通常由NO传感器(H-NOX或NosP蛋白)、传感器组氨酸蛋白激酶(histidine protein kinases, HPK)、含组氨酸的磷酸转移蛋白(His phosphotransmitter, HPt)和一种或多种响应调节蛋白组成,这些反应调节因子是具有PDE活性的效应蛋白或转录因子,如DipA、RbdA、NbdA等[51]。由于NO具有显著分散BF的能力,已被公认能与其他抗菌药联合使用治疗BAI,如与头孢菌素-3′-二氮鎓二酸盐和阿奇霉素、妥布霉素或环丙沙星联合用药,可有效清除非典型流感嗜血杆菌、铜绿假单胞菌、肺炎链球菌等的BF[52-54]。低剂量NO的辅助,还能增强妥布霉素(或头孢他啶和妥布霉素联合用药)清除囊性纤维化患者痰中铜绿假单胞菌BF[55]。
2 生物被膜分散剂的研发分散后的细菌耐药性大幅降低,这使得BAI的根除成为可能。因此,BF分散剂的研发逐渐受到重视。本课题组经过改良设计的鼠源抗微生物肽(cathelicidin related antimicrobial peptide, CRAMP)是一种潜在优良的BF分散剂,CRAMP能显著降低铜绿假单胞菌(实验室菌株PAO1) BF的c-di-GMP水平,并抑制EPS尤其是海藻酸钠(sodium alginate, ALG)的合成,还能促进细菌鞭毛的运动并增加RL的分泌[56-57];而且,CRAMP在联用万古霉素、罗红霉素和阿奇霉素时均表现出明显的协同作用,尤其是与万古霉素联用时,仅在3 h内并杀灭了全部(100%) BF[58]。同样有研究者发现CRAMP作为猪感染性结肠炎的免疫调节治疗,可增强肠道稳态,且未见CRAMP有毒副作用[59]。综上表明,CRAMP有望成为一种新型BF分散剂,以预防和控制未来人类或动物的BAI,但仍应探索CRAMP对不同微生物来源的BF的功效。
尽管BF的分散机制有待深入研究,但分散与基质降解相吻合的观点似乎已无异议。因此,许多研究者将具有高效降解BF基质能力的酶作为分散剂的发展对象,如DNase I、BlNucB (eDNA酶NucB的直系同源物)以及β-1, 3-糖苷酶等[60-62] (表 1)。有的则利用化学技术合成可与EPS直接作用的化合物,破坏EPS的结构,引起BF分散,如S-亚硝基谷胱甘肽(S-nitrosoglutathione, GSNO)、磁性氧化铁纳米颗粒(magnetic iron oxide nanoparticles, MNPs)、两性混合壳聚合物胶束(zwitterionic-mixed-shell polymeric micelles, ZW-MSPMs)等[63-65];亚油酸(linoleic acid, LA)、人内源性激素心房钠尿肽(human hormone atrial natriuretic peptide, hANP)等可通过抑制EPS中多糖和蛋白质合成,促使BF分散[66-67] (表 1)。在此,本文归纳了有望成为BF分散剂的物质(表 1)。
| No. | Item | Types of bacteria biofilm | Cause of BF dispersion |
| 1 | Synthesized cationic gemini surfactant (SCGS) | Sulfidogenic bacteria | SCGS inhibits the adhesive property of sulfidogenic bacteria biofilm cells on the metal surface[68] |
| 2 | Chlorhexidine gluconate (CHG) | Candida albicans | CHG inhibits the hyphal growth of C. albicans and disrupts the hyphal network in mature biofilm[69] |
| 3 | β-1, 3 glucanase | Candida albicans | β-1, 3-glucanase is able to degrade β-1, 3-glucan in EPS[62] |
| 4 | Zwitterionic, mixed-shell polymeric micelles (ZW-MSPMs) | Staphylococcus aureus | ZW-MSPMs interact strongly with eDNA and protein in EPS to disrupt the cohesion of biofilm[65] |
| 5 | Ce-metal organic framework (Ce-MoF) | Staphylococcus aureus | MOF/Ce can degrade eDNA in EPS[70] |
| 6 | 2-heptylcyclopropane-1-carboxylic acid (2CP) | Staphylococcus aureus, Pseudomonas aeruginosa |
2CP may not directly affect EPS but act at the cellular level[71] |
| 7 | Hydroxysteroid dehydro-genase 1835/1919 (HSD 1835, HSD 1919) | Staphylococcus aureus, Vancomycin-resistant Enterococci |
HSD 1835 or HSD 1919 is able to disrupt biofilm and inhibit the synthesis of DNA, RNA, protein and cell wall[72] |
| 8 | Linoleic acid (LA) | Staphylococcus aureus, Pseudomonas aeruginosa |
LA inhibits the synthesis of protein and polysaccharide in EPS[66] |
| 9 | Human atrial natriuretic peptide (hANP) | Pseudomonas aeruginosa | hANP inhibits the synthesis of polysaccharide in EPS significantly[67] |
| 10 | Iron-oxide nanoparticles (IONPs) | Pseudomonas aeruginosa | IONPs can release NO to disperse biofilm[73] |
| 11 | S-nitrosoglutathione (GSNO) | Pseudomonas aeruginosa, Acinetobacter baumannii | GSNO can simultaneously deliver GSH and NO to enhance biofilm dispersion[63] |
| 12 | Lipopeptide 6-2 | Pseudomonas aeruginosa, Bacillus cereus |
Lipopeptide6-2 inhibits the synthesis of Psl in EPS[74] |
| 13 | Modified nanoparticles (MNPs) | Methicillin-resistant Staphylococcus aureus | MNPs cause significant mechanical disruption to EPS and lead to biofilm dispersion[64] |
| 14 | Mesoporoussilica nanoparticles (MSNs) | Methicillin-resistant Staphylococcus aureus, Methicillin-susceptible Staphylococcus aureus |
MSNs can increase the efficacy of the enzymatic agent to degrade EPS[75] |
| 15 | Allyl piperidine-1-carbodiothioate (AP1C) | Mycobacterium smegmatis, Mycobacterium tuberculosis |
AP1C may inhibits the synthesis of proteins[76] |
| 16 | Benzyl 1H‐imidazole‐1‐carbodithioate and allyl piperidine‐1‐carbodioth ioate (B1HI1C) | Mycobacterium smegmatis, Mycobacterium tuberculosis |
B1HI1C may interfere with energy metabolism[76] |
| 17 | An unknown protein found in Bacillus subtilis is named NucB | Gram-negative bacteria, Gram-positive bacteria etc. |
BlNucB can degrade eDNA in EPS[61] |
| 18 | DNase I | Gram-negative bacteria, Gram-positive bacteria etc. |
DNase I degrades eDNA in EPS[60] |
| 19 | Paeonol | Klebsiella pneumoniae, Staphylococcus aureus, Enterobacter cloacae, Listeria monocytogenes |
Paeonol degrades eDNA, proteins and polysaccharides in EPS[77-78] |
| 20 | Proteinase K | Staphylococcus aureus | Proteinase K degrades eDNA and proteins in EPS[79] |
| 21 | Spermidine | Vibrio cholerae | Spermidine drops c-di-GMP levels of Vibrio cholerae cells and inhibits the synthesis of VPS in EPS[80] |
| 22 | 3, 5-dicaffeoylquinic acid (3, 5-DCQA) | Aspergillus Fumigatus | 3, 5-DCQA down-regulates the expression of hydrophobic genes[81] |
| 23 | Extracellular adenosine triphosphate (eATP) | Fusobacterium nucleatum | eATP chelates essential metal ions in F. nucleatum biofilm[82] |
| 24 | N-acetylgalactosaminidase Alpha (NAGa) | Desulfovibrio vulgaris, Desulfovibrio desulfuricans |
N-acetylgalactosaminidase can degrade GalNAc in EPS[83] |
| 25 | Dichloromethane-extractable carbon (DeoC) | Streptococcus mutans | DeoC promotes eDNA degradation in EPS[84] |
| 26 | BmdE protein | Propionibacterium acnes | BmdE is able to degrade eDNA in EPS[85] |
| 27 | Magnesium oxide nanoparticles (MgO-NPs) | Fusarium oxysporum | MgO NPs inhibits the synthesis of EPS significantly[86] |
| 28 | Enhalus acoroides leaf extract | Candida albicans, Escherichia coli |
The cause is not clear yet[87] |
| 29 | Mannose | Desulfovibrio vulgaris, desulfovibrio desulfuricans |
The cause is not clear yet[83] |
| 30 | 2-deoxy-d-glucose | Desulfovibrio vulgaris, desulfovibrio desulfuricans |
The cause is not clear yet[83] |
| 31 | Gold nanoparticles obtained from caffeine (Caff-AuNPs) | Gram-negative bacteria, Gram-positive bacteria etc. |
The cause is not clear yet[88] |
3 生物被膜分散后的潜在影响
有研究将分散后的细菌描述为一种介于BF细菌和浮游菌之间的表型,并与该两者相比表现出较大的差异性。首先,分散细菌具有高水平的表型异质性,考虑细菌本身较高的突变率,以及膜内细胞在应对不同微环境压力时不断分化的细胞亚群,这似乎是不难理解的,而且物种多样性的产生对于种群的存活与延续也具有重要意义。Guilhen等[89]利用RNAseq分析了肺炎克雷伯菌BF不同发育时期的转录组变化,结果发现:尽管分散细菌的转录组与7 h的BF转录组具有相似性,但仍显示出不同的转录谱;对比直系同源群的序列,亦发现分散的BF细菌具有更强的代谢能力。
其次,分散的细菌更具运动性、黏附性和毒性,这或许是分散细菌在为重新定植做准备。对流通池中白色念珠菌的RNA测序分析表明,与浮游菌相比,分散的酵母细菌表现出黏附性、侵袭性和BF形成能力增强[90]。而且分散的细菌能采用不同代谢方式,获取特定营养来代替碳源供能,与BF细菌相比,分散细菌中参与糖异生的基因表达增加[91]。在白色念珠菌颈静脉导管小鼠模型中,诱导BF分散,发现白色念珠菌对远端器官的感染能力增强了15倍[92];同样,分散的铜绿假单胞菌也显示出毒力增强[93]。有研究发现通过降低细菌内c-di-GMP水平,从BF中分散出的铜绿假单胞菌比浮游菌表现出更强的侵袭性与毒性,能杀死更多的巨噬细胞和秀丽隐杆线虫[91]。此外,有学者利用糖苷水解酶诱导小鼠体内铜绿假单胞菌与金黄色葡萄球菌BF分散,发现分散细菌导致小鼠全身性感染,部分小鼠则患败血症死亡[94]。以上研究对革兰阴性菌、阳性菌以及真菌中颇具代表的菌种进行了综述,其BF分散后的细菌均显示出毒力增强,并提示在今后研究中,应充分考虑BF分散后的细菌对于宿主或环境可能造成的影响。
4 展望BAI已越发受到人们的关注,研究者们也在不断地寻求能防治BAI的手段与方法,以往的研究大多围绕于如何抑制BF的形成或是直接杀灭BF细菌,如改造器械的表面性质(或添加涂层)以防止微生物的黏附,或是研发出新的强效抗菌药以清除(或渗入) BF并杀灭内部的细菌。但新的抗菌药总是会引发新的耐药问题,这使得BF在人或动物体内形成,导致的慢性感染始终得不到有效解决。分散,作为BF周期中少有关注,却又极为重要的一个环节,已引起研究者们的重视。分散后的细菌耐药性会呈指数倍下降,更易受到抗菌药与免疫反应的影响,而且分散剂作用于BF,或是干扰细菌内部的通讯传导,不直接杀灭细菌,可避免细菌耐药性的产生。因此,可将BF分散剂作为一种优良的抗菌药增效剂,与抗菌药联合使用达到控制BAI的目的,这也将成为医学领域研究的新热点。
BF分散往往伴随着BF基质的降解,这很可能与相关酶的合成有关,但还未有研究表明编码酶的基因是如何在感应到信号分子被激活。此外,对于BF内环境是如何影响亚群的形成与分散,BF内的亚群是否已做好准备分散;如果是,是怎样越过BF逃离出来的呢。将分散作为一种策略治疗BF引起的感染时,怎样的分散效率才能成为有效的分散剂。更为重要的是,目前对于分散的研究大都是基于单一病原的体外实验,但在临床中很少有微生物作为单一病原生长。为弥补这些研究中的差距,不仅需要探索大量单一病原和多物种病原体BF的分散,还需要在临床前和临床研究中探索分散与分散剂的作用,真正将分散的基础研究拓展到转化研究。
| [1] | DAVIES D. Understanding biofilm resistance to antibacterial agents[J]. Nature Reviews Drug Discovery, 2003, 2(2): 114-122 DOI:10.1038/nrd1008. |
| [2] | HELEEN VA, DIJCK PV, TOM C. Molecular mechanisms of antimicrobial tolerance and resistance in bacterial and fungal biofilms[J]. Trends in Microbiology, 2014, 22(6): 326-333 DOI:10.1016/j.tim.2014.02.001. |
| [3] | HØIBY N, BJARNSHOLT T, GIVSKOV M, MOLIN S, CIOFU O. Antibiotic resistance of bacterial biofilms[J]. International Journal of Antimicrobial Agents, 2010, 35(4): 322-332 DOI:10.1016/j.ijantimicag.2009.12.011. |
| [4] | del POZO JL. Biofilm-related disease[J]. Expert Review of Anti-Infective Therapy, 2018, 16(1): 51-65 DOI:10.1080/14787210.2018.1417036. |
| [5] | TOLKER-NIELSEN T. Biofilm development[J]. Microbiology Spectrum, 2015, 3(2): MB-0001-2014. |
| [6] | RUMBAUGH KP, SAUER K. Biofilm dispersion[J]. Nature Reviews Microbiology, 2020, 18(10): 571-586 DOI:10.1038/s41579-020-0385-0. |
| [7] | PETROVA OE, SAUER K. Escaping the biofilm in more than one way: desorption, detachment or dispersion[J]. Current Opinion in Microbiology, 2016, 30: 67-78 DOI:10.1016/j.mib.2016.01.004. |
| [8] | LEE SW, GU H, KILBERG JB, REN DC. Sensitizing bacterial cells to antibiotics by shape recovery triggered biofilm dispersion[J]. Acta Biomaterialia, 2018, 81: 93-102 DOI:10.1016/j.actbio.2018.09.042. |
| [9] | DAVIES DG, MARQUES CNH. A fatty acid messenger is responsible for inducing dispersion in microbial biofilms[J]. Journal of Bacteriology, 2009, 191(5): 1393-1403 DOI:10.1128/JB.01214-08. |
| [10] | VALENTIN JDP, STRAUB H, PIETSCH F, LEMARE M, AHRENS CH, SCHREIBER F, WEBB JS, van der MEI HC, REN Q. Role of the flagellar hook in the structural development and antibiotic tolerance of Pseudomonas aeruginosa biofilms[J]. The ISME Journal, 2022, 16(4): 1176-1186 DOI:10.1038/s41396-021-01157-9. |
| [11] | RÖMLING U, GALPERIN MY. Discovery of the second messenger cyclic di-GMP[M]//c-di-GMP Signaling. New York, NY: Springer New York, 2017: 1-8. |
| [12] | JUNKERMEIER EH, HENGGE R. A novel locally c-di-GMP-controlled exopolysaccharide synthase required for bacteriophage N4 infection of Escherichia coli[J]. mBio, 2021, 12(6): 1-18. |
| [13] | ELGAMOUDI BA, STARR KS, KOROLIK V. Extracellular c-di-GMP plays a role in biofilm formation and dispersion of Campylobacter jejuni[J]. Microorganisms, 2022, 10(10): 2030 DOI:10.3390/microorganisms10102030. |
| [14] | SARENKO O, KLAUCK G, WILKE FM, PFIFFER V, RICHTER AM, HERBST S, KAEVER V, HENGGE R. More than enzymes that make or break cyclic di-GMP—local signaling in the interactome of GGDEF/EAL domain proteins of Escherichia coli[J]. mBio, 2017, 8(5): 1-18. |
| [15] | LIU C, LIEW CW, WONG YH, TAN ST, POH WH, MANIMEKALAI MSS, RAJAN S, XIN LY, LIANG ZX, GRÜBER G, RICE SA, LESCAR J. Insights into biofilm dispersal regulation from the crystal structure of the PAS-GGDEF-EAL region of RbdA from Pseudomonas aeruginosa[J]. Journal of Bacteriology, 2018, 200(3): 1-19. |
| [16] | XU GG, ZHOU LC, QIAN GL, LIU FQ. Diguanylate cyclase and phosphodiesterase interact to maintain the specificity of cyclic di-GMP signaling in the regulation of antibiotic synthesis in Lysobacter enzymogenes[J]. Applied and Environmental Microbiology, 2022, 88(2): 1-13. |
| [17] | LIN SY, CHEN SZ, LI L, CAO HL, LI T, HU M, LIAO LS, ZHANG LH, XU ZL. Genome characterization of a uropathogenic Pseudomonas aeruginosa isolate PA_HN002 with cyclic di-GMP-dependent hyper-biofilm production[J]. Frontiers in Cellular and Infection Microbiology, 2022, 12: 1-15. |
| [18] | FUQUA C, GREENBERG EP. Listening in on bacteria: acyl-homoserine lactone signalling[J]. Nature Reviews Molecular Cell Biology, 2002, 3(9): 685-695 DOI:10.1038/nrm907. |
| [19] | ABISADO RG, BENOMAR S, KLAUS JR, DANDEKAR AA, CHANDLER JR. Bacterial quorum sensing and microbial community interactions[J]. mBio, 2018, 9(3): e02331-e02317. |
| [20] | SU JH, ZHANG Q, HUANG WS, SONG JY, PENG HJ, FENG JP, HE J, ZHANG YJ, WEI HUA. Transfer of functional microorganism: regulation of N-acyl-homoserine lactones on the microbial community in aniline-degrading sequencing batch biofilm reactor[J]. Bioresource Technology, 2022, 351: 1-9. |
| [21] | WANG JF, LIU QJ, DONG DY, HU HD, WU B, REN HQ. AHLs-mediated quorum sensing threshold and its response towards initial adhesion of wastewater biofilms[J]. Water Research, 2021, 194: 1-10. |
| [22] | UEDA A, WOOD TK. Connecting quorum sensing, c-di-GMP, pel polysaccharide, and biofilm formation in Pseudomonas aeruginosa through tyrosine phosphatase TpbA (PA3885)[J]. PLoS Pathogens, 2009, 5(6): e1000483 DOI:10.1371/journal.ppat.1000483. |
| [23] | GUPTA R, SCHUSTER M. Quorum sensing modulates colony morphology through alkyl quinolones in Pseudomonas aeruginosa[J]. BMC Microbiology, 2012, 12: 30 DOI:10.1186/1471-2180-12-30. |
| [24] | ZAHIDULLAH, SIDDIQUI MF, TABRAIZ S, MAQBOOL F, ADNAN F, ULLAH I, SHAH MA, JADOON WA, MEHMOOD T, QAYYUM S, RAHMAN Z. Targeting microbial biofouling by controlling biofilm formation and dispersal using rhamnolipids on RO membrane[J]. Membranes, 2022, 12(10): 928 DOI:10.3390/membranes12100928. |
| [25] | WOOD TL, GONG T, ZHU L, MILLER J, MILLER DS, YIN B, WOOD TK. Rhamnolipids from Pseudomonas aeruginosa disperse the biofilms of sulfate-reducing bacteria[J]. Npj Biofilms and Microbiomes, 2018, 4: 22 DOI:10.1038/s41522-018-0066-1. |
| [26] | BHATTACHARJEE A, NUSCA TD, HOCHBAUM AI. Rhamnolipids mediate an interspecies biofilm dispersal signaling pathway[J]. ACS Chemical Biology, 2016, 11(11): 3068-3076 DOI:10.1021/acschembio.6b00750. |
| [27] | PESCI EC, MILBANK JB, PEARSON JP, MCKNIGHT S, KENDE AS, GREENBERG EP, IGLEWSKI BH. Quinolone signaling in the cell-to-cell communication system of Pseudomonas aeruginosa[J]. Proceedings of the National Academy of Sciences of the United States of America, 1999, 96(20): 11229-11234. |
| [28] | THORNHILL SG, MCLEAN RJC. Use of whole-cell bioassays for screening quorum signaling, quorum interference, and biofilm dispersion[M]//Methods in Molecular Biology. New York, NY: Springer New York, 2017: 3-24. |
| [29] | RAMPIONI G, FALCONE M, HEEB S, FRANGIPANI E, FLETCHER MP, DUBERN JF, VISCA P, LEONI L, CÁMARA M, WILLIAMS P. Unravelling the genome-wide contributions of specific 2-alkyl-4-quinolones and PqsE to quorum sensing in Pseudomonas aeruginosa[J]. PLoS Pathogens, 2016, 12(11): e1006029 DOI:10.1371/journal.ppat.1006029. |
| [30] | LIN CS, LIU Y, LI YY, TING HJ, KOHLI GS, CAI Z, SUWANCHAIKASEM P, KAU KIT GOH K, PIN NG S, TOLKER-NIELSEN T, YANG L, GIVSKOV M. Reduced intracellular c-di-GMP content increases expression of quorum sensing-regulated genes in Pseudomonas aeruginosa[J]. Frontiers in Cellular and Infection Microbiology, 2017, 7: 451 DOI:10.3389/fcimb.2017.00451. |
| [31] | COOKE AC, FLOREZ C, DUNSHEE EB, LIEBER AD, TERRY ML, LIGHT CJ, SCHERTZER JW. Pseudomonas quinolone signal-induced outer membrane vesicles enhance biofilm dispersion in Pseudomonas aeruginosa[J]. mSphere, 2020, 5(6): e01109-20. |
| [32] | HE YW, DENG YY, MIAO YS, CHATTERJEE S, TRAN TM, TIAN J, LINDOW S. DSF-family quorum sensing signal-mediated intraspecies, interspecies, and inter-kingdom communication[J]. Trends in Microbiology, 2023, 31(1): 36-50 DOI:10.1016/j.tim.2022.07.006. |
| [33] | WANG FF, QIAN W. The roles of histidine kinases in sensing host plant and cell-cell communication signal in a phytopathogenic bacterium[J]. Philosophical Transactions of the Royal Society B: Biological Sciences, 2019, 374(1767): 20180311 DOI:10.1098/rstb.2018.0311. |
| [34] | TAO F, SWARUP S, ZHANG LH. Quorum sensing modulation of a putative glycosyltransferase gene cluster essential for Xanthomonas campestris biofilm formation[J]. Environmental Microbiology, 2010, 12(12): 3159-3170 DOI:10.1111/j.1462-2920.2010.02288.x. |
| [35] | TIAN XQ, WU Y, CAI Z, QIAN W. BDSF is a degradation-prone quorum-sensing signal detected by the histidine kinase RpfC of Xanthomonas campestris pv. campestris[J]. Applied and Environmental Microbiology, 2022, 88(8): e0003122 DOI:10.1128/aem.00031-22. |
| [36] | WEST KHJ, SHEN WQ, EISENBRAUN EL, YANG T, VASQUEZ JK, HORSWILL AR, BLACKWELL HE. Non-native peptides capable of pan-activating the agr quorum sensing system across multiple specificity groups of Staphylococcus epidermidis[J]. ACS Chemical Biology, 2021, 16(6): 1070-1078 DOI:10.1021/acschembio.1c00240. |
| [37] | SRIVASTAVA SK, RAJASREE K, FASIM A, ARAKERE G, GOPAL B. Influence of the AgrC-AgrA complex on the response time of Staphylococcus aureus quorum sensing[J]. Journal of Bacteriology, 2014, 196(15): 2876-2888 DOI:10.1128/JB.01530-14. |
| [38] | BRIDGES AA, BASSLER BL. The intragenus and interspecies quorum-sensing autoinducers exert distinct control over Vibrio cholerae biofilm formation and dispersal[J]. PLoS Biology, 2019, 17(11): e3000429 DOI:10.1371/journal.pbio.3000429. |
| [39] | DÍAZ-SALAZAR C, CALERO P, ESPINOSA-PORTERO R, JIMÉNEZ-FERNÁNDEZ A, WIREBRAND L, VELASCO-DOMÍNGUEZ MG, LÓPEZ-SÁNCHEZ A, SHINGLER V, GOVANTES F. The stringent response promotes biofilm dispersal in Pseudomonas putida[J]. Scientific Reports, 2017, 7: 18055 DOI:10.1038/s41598-017-18518-0. |
| [40] | PENG JY, SCHACHTERLE JK, SUNDIN GW. Orchestration of virulence factor expression and modulation of biofilm dispersal in Erwinia amylovorathrough activation of the Hfq-dependent small RNA RprA[J]. Molecular Plant Pathology, 2021, 22(2): 255-270 DOI:10.1111/mpp.13024. |
| [41] | GOODWINE J, GIL J, DOIRON A, VALDES J, SOLIS M, HIGA A, DAVIS S, SAUER K. Pyruvate-depleting conditions induce biofilm dispersion and enhance the efficacy of antibiotics in killing biofilms in vitro and in vivo[J]. Scientific Reports, 2019, 9: 3763 DOI:10.1038/s41598-019-40378-z. |
| [42] | MCDONOUGH E, KAMP H, CAMILLI A. Vibrio cholerae phosphatases required for the utilization of nucleotides and extracellular DNAas phosphate sources[J]. Molecular Microbiology, 2016, 99(3): 453-469 DOI:10.1111/mmi.13128. |
| [43] | ZHU XY, RICE SA, BARRAUD N. Nitric oxide and iron signaling cues have opposing effects on biofilm development in Pseudomonas aeruginosa[J]. Applied and Environmental Microbiology, 2019, 85(3): e02175-18. |
| [44] | SAUER K, CULLEN MC, RICKARD AH, ZEEF LAH, DAVIES DG, GILBERT P. Characterization of nutrient-induced dispersion in Pseudomonas aeruginosa PAO1 biofilm[J]. Journal of Bacteriology, 2004, 186(21): 7312-7326 DOI:10.1128/JB.186.21.7312-7326.2004. |
| [45] | UPPULURI P, CHATURVEDI AK, SRINIVASAN A, BANERJEE M, RAMASUBRAMANIAM AK, KÖHLER JR, KADOSH D, LOPEZ-RIBOT JL. Dispersion as an important step in the Candida albicans biofilm developmental cycle[J]. PLoS Pathogens, 2010, 6(3): e1000828 DOI:10.1371/journal.ppat.1000828. |
| [46] | HUYNH TT, MCDOUGALD D, KLEBENSBERGER J, AL QARNI B, BARRAUD N, RICE SA, KJELLEBERG S, SCHLEHECK D. Glucose starvation-induced dispersal of Pseudomonas aeruginosa biofilms is cAMP and energy dependent[J]. PLoS One, 2012, 7(8): e42874 DOI:10.1371/journal.pone.0042874. |
| [47] | SINGH PK, BARTALOMEJ S, HARTMANN R, JECKEL H, VIDAKOVIC L, NADELL CD, DRESCHER K. Vibrio cholerae combines individual and collective sensing to trigger biofilm dispersal[J]. Current Biology, 2017, 27(21): 3359-3366.e7 DOI:10.1016/j.cub.2017.09.041. |
| [48] | BARRAUD N, STOREY MV, MOORE ZP, WEBB JS, RICE SA, KJELLEBERG S. Nitric oxide-mediated dispersal in single- and multi-species biofilms of clinically and industrially relevant microorganisms[J]. Microbial Biotechnology, 2009, 2(3): 370-378 DOI:10.1111/j.1751-7915.2009.00098.x. |
| [49] | BARRAUD N, HASSETT DJ, HWANG SH, RICE SA, KJELLEBERG S, WEBB JS. Involvement of nitric oxide in biofilm dispersal of Pseudomonas aeruginosa[J]. Journal of Bacteriology, 2006, 188(21): 7344-7353 DOI:10.1128/JB.00779-06. |
| [50] | ZHANG GJ, YANG Z, ZHOU YC, ZHU DZ, ZHANG YP, YU T, SHYPANSKI A. Combination of nitrate and sodium nitroprusside dosing for sulfide control with low carbon source loss in sewer biofilm reactors[J]. Journal of Hazardous Materials, 2022, 424: 127527 DOI:10.1016/j.jhazmat.2021.127527. |
| [51] | WILLIAMS DE, BOON EM. Towards understanding the molecular basis of nitric oxide-regulated group behaviors in pathogenic bacteria[J]. Journal of Innate Immunity, 2019, 11(3): 205-215 DOI:10.1159/000494740. |
| [52] | COLLINS SA, KELSO MJ, RINEH A, YEPURI NR, COLES J, JACKSON CL, HALLADAY GD, WALKER WT, WEBB JS, HALL-STOODLEY L, CONNETT GJ, FEELISCH M, FAUST SN, LUCAS JSA, ALLAN RN. Cephalosporin-3′-diazeniumdiolate NO donor prodrug PYRRO-C3D enhances azithromycin susceptibility of nontypeable Haemophilus influenzae biofilms[J]. Antimicrobial Agents and Chemotherapy, 2017, 61(2): e02086-16. |
| [53] | BARRAUD N, KARDAK BG, YEPURI NR, HOWLIN RP, WEBB JS, FAUST SN, KJELLEBERG S, RICE SA, KELSO MJ. Cephalosporin-3′-diazeniumdiolates: targeted NO-donor prodrugs for dispersing bacterial biofilms[J]. Angewandte Chemie International Edition, 2012, 51(36): 9057-9060 DOI:10.1002/anie.201202414. |
| [54] | ALLAN RN, KELSO MJ, RINEH A, YEPURI NR, FEELISCH M, SOREN O, BRITO-MUTUNAYAGAM S, SALIB RJ, STOODLEY P, CLARKE SC, WEBB JS, HALL-STOODLEY L, FAUST SN. Cephalosporin-NO-donor prodrug PYRRO-C3D shows β-lactam-mediated activity against Streptococcus pneumoniae biofilms[J]. Nitric Oxide, 2017, 65: 43-49 DOI:10.1016/j.niox.2017.02.006. |
| [55] | HOWLIN RP, CATHIE K, HALL-STOODLEY L, CORNELIUS V, DUIGNAN C, ALLAN RN, FERNANDEZ BO, BARRAUD N, BRUCE KD, JEFFERIES J, KELSO M, KJELLEBERG S, RICE SA, ROGERS GB, PINK S, SMITH C, SUKHTANKAR PS, SALIB R, LEGG J, CARROLL M, et al. Low-dose nitric oxide as targeted anti-biofilm adjunctive therapy to treat chronic Pseudomonas aeruginosa infection in cystic fibrosis[J]. Molecular Therapy, 2017, 25(9): 2104-2116 DOI:10.1016/j.ymthe.2017.06.021. |
| [56] | ZHANG Y, CHENG P, WANG SY, LI XF, PENG LC, FANG RD, XIONG J, LI H, MEI C, GAO JY, SONG ZH, XU DF, FU LZ, LI CH, WU XQ, HE YZ, CHEN HW. Pseudomonas aeruginosa biofilm dispersion by the mouse antimicrobial peptide CRAMP[J]. Veterinary Research, 2022, 53(1): 80 DOI:10.1186/s13567-022-01097-y. |
| [57] |
张阳, 程鹏, 熊静, 李晓芬, 李会, 王士源, 彭练慈, 韩玉竹, 刘娟, 陈红伟. 基于RNA-Seq技术分析鼠源宿主防御肽对铜绿假单胞菌成熟生物被膜的清除作用[J]. 微生物学报, 2021, 61(9): 2843-2853.
ZHANG Y, CHENG P, XIONG J, LI XF, LI H, WANG SY, PENG LC, HAN YZ, LIU J, CHEN HW. Eradication effect of Pseudomonas aeruginosa biofilms by mouse host defense peptide based on RNA-Seq technology[J]. Acta Microbiologica Sinica, 2021, 61(9): 2843-2853 (in Chinese). |
| [58] |
熊静, 王士源, 李会, 张阳, 程鹏, 梅翠, 彭练慈, 徐登峰, 高继业, 何玉张, 陈红伟. 抗微生物肽CRAMP联合抗生素分散铜绿假单胞菌生物被膜的增效作用研究[J]. 微生物学报, 2022, 62(8): 3251-3262.
XIONG J, WANG SY, LI H, ZHANG Y, CHENG P, MEI C, PENG LC, XU DF, GAO JY, HE YZ, CHEN HW. Synergistic effect of CRAMP and antibiotic against Pseudomonas aeruginosa biofilm[J]. Acta Microbiologica Sinica, 2022, 62(8): 3251-3262 (in Chinese). |
| [59] | CRISTINA CF, ROBERT MC, GREG M, EDUARDO RC. Systemic murine cathelicidin CRAMP safely attenuated colonic neutrophil infiltration in pigs[J]. Veterinary Immunology and Immunopathology, 2022, 249: 110443 DOI:10.1016/j.vetimm.2022.110443. |
| [60] | OKSHEVSKY M, REGINA VR, MEYER RL. Extracellular DNA as a target for biofilm control[J]. Current Opinion in Biotechnology, 2015, 33: 73-80 DOI:10.1016/j.copbio.2014.12.002. |
| [61] | BASLÉ A, HEWITT L, KOH A, LAMB HK, THOMPSON P, BURGESS JG, HALL MJ, HAWKINS AR, MURRAY H, LEWIS RJ. Crystal structure of NucB, a biofilm-degrading endonuclease[J]. Nucleic Acids Research, 2018, 46(1): 473-484 DOI:10.1093/nar/gkx1170. |
| [62] | TAN YL, MA S, LEONHARD M, MOSER D, SCHNEIDER-STICKLER B. β-1, 3-glucanase disrupts biofilm formation and increases antifungal susceptibility of Candida albicans DAY185[J]. International Journal of Biological Macromolecules, 2018, 108: 942-946 DOI:10.1016/j.ijbiomac.2017.11.003. |
| [63] | DAS T, CHOONG HJ, KWANG YC, CHAN HK, MANOS J, KWOK PCL, DUONG HTT. Spray-dried particles of nitric oxide-modified glutathione for the treatment of chronic lung infection[J]. Molecular Pharmaceutics, 2019, 16(4): 1723-1731 DOI:10.1021/acs.molpharmaceut.9b00080. |
| [64] | LI J, NICKEL R, WU JD, LIN F, van LIEROP J, LIU S. A new tool to attack biofilms: driving magnetic iron-oxide nanoparticles to disrupt the matrix[J]. Nanoscale, 2019, 11(14): 6905-6915 DOI:10.1039/C8NR09802F. |
| [65] | TIAN S, SU LZ, LIU Y, CAO JJ, YANG G, REN YJ, HUANG F, LIU JF, AN YL, van der MEI HC, BUSSCHER HJ, SHI LQ. Self-targeting, zwitterionic micellar dispersants enhance antibiotic killing of infectious biofilms-an intravital imaging study in mice[J]. Science Advances, 2020, 6(33): eabb1112 DOI:10.1126/sciadv.abb1112. |
| [66] | HAM SY, KIM HS, JANG Y, RYOO HS, LEE JH, PARK JH, PARK HD. Synergistic control of membrane biofouling using linoleic acid and sodium hypochlorite[J]. Chemosphere, 2021, 268: 128802 DOI:10.1016/j.chemosphere.2020.128802. |
| [67] | LOUIS M, CLAMENS T, TAHRIOUI A, DESRIAC F, RODRIGUES S, ROSAY T, HARMER N, DIAZ S, BARREAU M, RACINE PJ, KIPNIS E, GRANDJEAN T, VIEILLARD J, BOUFFARTIGUES E, CORNELIS P, CHEVALIER S, FEUILLOLEY MGJ, LESOUHAITIER O. Pseudomonas aeruginosa biofilm dispersion by the human atrial natriuretic peptide[J]. Advanced Science, 2022, 9(7): 2103262 DOI:10.1002/advs.202103262. |
| [68] | LABENA A, HEGAZY MA, SAMI RM, HOZZEIN WN. Multiple applications of a novel cationic gemini surfactant: anti-microbial, anti-biofilm, biocide, salinity corrosion inhibitor, and biofilm dispersion (part Ⅱ)[J]. Molecules, 2020, 25(6): 1348 DOI:10.3390/molecules25061348. |
| [69] | ALVENDAL C, MOHANTY S, BOHM-STARKE N, BRAUNER A. Anti-biofilm activity of chlorhexidine digluconate against Candida albicans vaginal isolates[J]. PLoS One, 2020, 15(9): e0238428 DOI:10.1371/journal.pone.0238428. |
| [70] | LIU ZW, WANG F, REN JS, QU XG. A series of MOF/Ce-based nanozymes with dual enzyme-like activity disrupting biofilms and hindering recolonization of bacteria[J]. Biomaterials, 2019, 208: 21-31 DOI:10.1016/j.biomaterials.2019.04.007. |
| [71] | HARRISON ZL, AWAIS R, HARRIS M, RAJI B, HOFFMAN BC, BAKER DL, JENNINGS JA. 2-heptylcyclopropane-1-carboxylic acid disperses and inhibits bacterial biofilms[J]. Frontiers in Microbiology, 2021, 12: 645180 DOI:10.3389/fmicb.2021.645180. |
| [72] | DAYAL NT, ONYEDIBE KI, GRIBBLE WM, SINTIM HO. Membrane acting Povarov-Doebner derived compounds potently disperse preformed multidrug resistant Gram-positive bacterial biofilms[J]. European Journal of Medicinal Chemistry, 2022, 240: 114550 DOI:10.1016/j.ejmech.2022.114550. |
| [73] | ADNAN NNM, SADREARHAMI Z, BAGHERI A, NGUYEN TK, WONG EHH, HO KKK, LIM M, KUMAR N, BOYER C. Exploiting the versatility of polydopamine-coated nanoparticles to deliver nitric oxide and combat bacterial biofilm[J]. Macromolecular Rapid Communications, 2018, 39(13): 1800159 DOI:10.1002/marc.201800159. |
| [74] | SONG B, WANG YZ, WANG GY, LIU GL, LI WZ, YAN F. The lipopeptide 6-2 produced by Bacillus amyloliquefaciens anti-CA has potent activity against the biofilm-forming organisms[J]. Marine Pollution Bulletin, 2016, 108(1/2): 62-69. |
| [75] | DEVLIN H, FULAZ S, HIEBNER DW, O'GARA JP, CASEY E. Enzyme-functionalized mesoporous silica nanoparticles to target Staphylococcus aureus and disperse biofilms[J]. International Journal of Nanomedicine, 2021, 16: 1929-1942 DOI:10.2147/IJN.S293190. |
| [76] | MUKHERJEE G, MUKHERJEE K, DAS R, MANDAL RS, ROY I, MUKHOPADHYAY B, SIL AK. Allyl piperidine-1-carbodiothioate and benzyl 1H-imidazole 1 carbodithioate: two potential agents to combat against mycobacteria[J]. Journal of Applied Microbiology, 2021, 130(3): 786-796 DOI:10.1111/jam.14762. |
| [77] | QIAN WD, LI XC, YANG M, MAO GN. Antibacterial and anti-biofilm activities of paeonol against Klebsiella pneumoniae and Enterobacter cloacae[J]. Biofouling, 2021, 37(6): 666-679 DOI:10.1080/08927014.2021.1955249. |
| [78] | ZENG Q, FU YT, YANG M, WANG T, WANG Y, LV SH, QIAN WD. Effect of paeonol against bacterial growth, biofilm formation and dispersal of Staphylococcus aureus and Listeria monocytogenes in vitro[J]. Biofouling, 2022, 38(2): 173-185 DOI:10.1080/08927014.2022.2045014. |
| [79] | RAO T, SHUKLA S. Staphylococcus aureus biofilm removal by targeting biofilm-associated extracellular proteins[J]. Indian Journal of Medical Research, 2017, 146(7): 1 DOI:10.4103/ijmr.IJMR_410_15. |
| [80] | BRIDGES AA, BASSLER BL. Inverse regulation of Vibrio cholerae biofilm dispersal by polyamine signals[J]. eLife, 2021, 10: 65487 DOI:10.7554/eLife.65487. |
| [81] | LUO J, WANG K, LI GS, LEI DQ, HUANG YJ, LI WD, CHEN YQ, KONG JL. 3, 5-dicaffeoylquinic acid disperses Aspergillus fumigatus biofilm and enhances fungicidal efficacy of voriconazole and amphotericin B[J]. Medical Science Monitor, 2018, 24: 427-437 DOI:10.12659/MSM.908068. |
| [82] | DING QF, TAN KS. The danger signal extracellular ATP is an inducer of Fusobacterium nucleatum biofilm dispersal[J]. Frontiers in Cellular and Infection Microbiology, 2016, 6: 155. |
| [83] | POOSARLA VG, WOOD TL, ZHU L, MILLER DS, YIN B, WOOD TK. Dispersal and inhibitory roles of mannose, 2-deoxy-d-glucose and N-acetylgalactosaminidase on the biofilm of Desulfovibrio vulgaris[J]. Environmental Microbiology Reports, 2017, 9(6): 779-787 DOI:10.1111/1758-2229.12595. |
| [84] | LIU J, SUN LP, LIU W, GUO LH, LIU ZH, WEI X, LING JQ. A nuclease from Streptococcus mutans facilitates biofilm dispersal and escape from killing by neutrophil extracellular traps[J]. Frontiers in Cellular and Infection Microbiology, 2017, 7: 97. |
| [85] | BRONNEC V, EILERS H, JAHNS AC, OMER H, ALEXEYEV OA. Propionibacterium (Cutibacterium) granulosum extracellular DNase BmdE targeting Propionibacterium (Cutibacterium) acnes biofilm matrix, a novel inter-species competition mechanism[J]. Frontiers in Cellular and Infection Microbiology, 2022, 11: 809792 DOI:10.3389/fcimb.2021.809792. |
| [86] | ABDEL-AZIZ MM, EMAM TM, ELSHERBINY EA. Bioactivity of magnesium oxide nanoparticles synthesized from cell filtrate of Endobacterium Burkholderia rinojensis against Fusarium oxysporum[J]. Materials Science and Engineering: C, 2020, 109: 110617 DOI:10.1016/j.msec.2019.110617. |
| [87] | de VL, GLASENAPP Y, CATTÒ C, VILLA F, CAPPITELLI F, PAPENBROCK J. Hindering the formation and promoting the dispersion of medical biofilms: non-lethal effects of seagrass extracts[J]. BMC Complementary and Alternative Medicine, 2018, 18(1): 1-17 DOI:10.1186/s12906-017-2057-9. |
| [88] | KHAN F, PARK SK, BAMUNUARACHCHI NI, OH D, KIM YM. Caffeine-loaded gold nanoparticles: antibiofilm and anti-persister activities against pathogenic bacteria[J]. Applied Microbiology and Biotechnology, 2021, 105(9): 3717-3731 DOI:10.1007/s00253-021-11300-3. |
| [89] | GUILHEN C, CHARBONNEL N, PARISOT N, GUEGUEN N, ILTIS A, FORESTIER C, BALESTRINO D. Transcriptional profiling of Klebsiella pneumoniae defines signatures for planktonic, sessile and biofilm-dispersed cells[J]. BMC Genomics, 2016, 17: 237 DOI:10.1186/s12864-016-2557-x. |
| [90] | WU JD, WU DQ, ZHAO YY, SI YQ, MEI LF, SHAO J, WANG TM, YAN GM, WANG CZ. Sodium new houttuyfonate inhibits Candida albicans biofilm formation by inhibiting the Ras1-cAMP-Efg1 pathway revealed by RNA-seq[J]. Frontiers in Microbiology, 2020, 11: 2075 DOI:10.3389/fmicb.2020.02075. |
| [91] | CHUA SL, LIU Y, YAM JKH, CHEN YC, VEJBORG RM, TAN BGC, KJELLEBERG S, TOLKER-NIELSEN T, GIVSKOV M, YANG L. Dispersed cells represent a distinct stage in the transition from bacterial biofilm to planktonic lifestyles[J]. Nature Communications, 2014, 5: 4462 DOI:10.1038/ncomms5462. |
| [92] | UPPULURI P, ACOSTA ZALDÍVAR M, ANDERSON MZ, DUNN MJ, BERMAN J, LOPEZ RIBOT JL, KÖHLER JR. Candida albicans dispersed cells are developmentally distinct from biofilm and planktonic cells[J]. mBio, 2018, 9(4): e01338-18. |
| [93] | HWANG HJ, LI XH, KIM SK, LEE JH. Anthranilate acts as a signal to modulate biofilm formation, virulence, and antibiotic tolerance of Pseudomonas aeruginosa and surrounding bacteria[J]. Microbiology Spectrum, 2022, 10(1): e0146321 DOI:10.1128/spectrum.01463-21. |
| [94] | FLEMING D, RUMBAUGH K. The consequences of biofilm dispersal on the host[J]. Scientific Reports, 2018, 8: 10738 DOI:10.1038/s41598-018-29121-2. |
 2023, Vol. 63
2023, Vol. 63




